Is the public being told the truth about new bunionectomy procedures?
Several foot and ankle surgical companies such as Arthrex, Crossroads, Paragon 28, and Treace Medical are marketing direct to the consumer on the internet to promote their technologies while also featuring “Find a Doctor” tools .
Of concern, two surgical companies are marketing directly to consumers (patients) on the internet and touting questionable advantages of “3-D and 4-D” correction of bunions utilizing a modified Lapidus procedure. Practitioners are now reporting frustration with having to defend their recommendation of traditional surgical procedures for hallux valgus deformity (HAV) when patients confront them with un-substantiated claims which they read on the internet posted by surgical companies. (1)
Let’s take a deep dive and see if the claims made by surgical companies on the internet about the superiority of “3-D or 4-D” bunion correction really hold up to scientific scrutiny.
Claim #1: Addressing the “Root Cause” of the bunion while all other procedures do not.
A central theme is posted on the Treace Medical website promoting the Lapiplasty® procedure (2):
“Patented advanced technology designed to correct all three dimensions of the bunion at the root of the problem ( unstable joint). While the majority of bunion surgery is only 2D and fails to address the root cause, Lapiplasty® provides a 3D correction and secures the unstable joint. “
Fusion Orthopedics makes a similar claim in their advertising of the LapiLock bunionectomy procedure (3):
“A root cause of some bunions is the genetically unstable cuneiform joint, which often remains uncorrected!”
FACT: There is no credible evidence that an unstable first metatarsocuneiform joint precedes or causes hallux valgus deformity.
Published research shows that instability of the first metatarsocuneiform joint in all thee planes is the result of, not the cause of HAV deformity. (4-8)
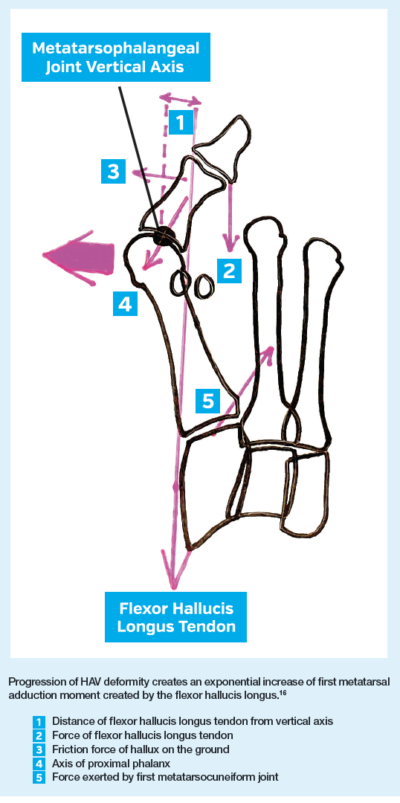 In a pivotal study, Munuera and co-workers evaluated 49 patients with early onset of hallux valgus deformity and compared radiographic measures to 49 healthy controls.(9) While lateral deviation of the hallux was present only in the HAV group, an insignificant difference of intermetatarsal angle (1-2 IMA) was shown in both groups. Munera and co-workers concluded that medial deviation of the first metatarsal which is shown in progressive HAV deformity occurs as a result of lateral deviation of the hallux. They cite the works of Sanders and Snijders who used cadaver models to demonstrate the powerful mechanical effect of a deviated hallux on the more proximal located first metatarsocuneiform joint.(10,11)
In a pivotal study, Munuera and co-workers evaluated 49 patients with early onset of hallux valgus deformity and compared radiographic measures to 49 healthy controls.(9) While lateral deviation of the hallux was present only in the HAV group, an insignificant difference of intermetatarsal angle (1-2 IMA) was shown in both groups. Munera and co-workers concluded that medial deviation of the first metatarsal which is shown in progressive HAV deformity occurs as a result of lateral deviation of the hallux. They cite the works of Sanders and Snijders who used cadaver models to demonstrate the powerful mechanical effect of a deviated hallux on the more proximal located first metatarsocuneiform joint.(10,11)
Ironically, Paul Dayton who is a co-owner of the patent for the Lapiplasty® procedure published a paper citing the research of Munuera et al and Snijders et al and supported the theory that the hallux, not the first metatarsocuneiform joint, was the driving force of HAV deformity. (12) In his cadaver study, Dayton showed how lateral deviation of the hallux caused retrograde medial deviation of the first metatarsal and concluded:
“From these observations, it is possible that the hallux could drive the proximal changes in the first ray that lead to metatarsus primus adducto valgus deformity.”
Clearly these studies support the notion that lateral deviation of the hallux is the actual event preceding medial deviation of the first metatarsocuneiform joint. The root cause of the bunion begins with the hallux and the instability of the first metatarsocuneiform joint is a secondary finding.
Claim #2: Hallux valgus surgery requires correction of the “third dimension” of the bunion deformity.
From the Lapiplasty® website (2):
“80% of bunions are misaligned in 3 dimensions”
“12 x likelihood of bunion returning if the 3D problem isn’t addressed”
FACT: A pronated position of the first metatarsal is not peculiar to hallux valgus
The so-called third dimension of the bunion deformity was described by Lapiplasty pioneer Paul Dayton in 2014, who cited previous literature describing an everted position of the first metatarsal to the ground in HAV patients. (13) Subsequently, several studies showed that an everted or pronated position of the first metatarsal is not peculiar to hallux valgus deformity, but is a result of whole foot pronation.(14,15)
A pronated position of the first metatarsal is found in patients without hallux valgus deformity. (16,17) The notion that pronation of the first metatarsal directly causes hallux valgus deformity is dispelled by studies showing that there is no direct relationship between the severity of hallux valgus deformity and the magnitude of first metatarsal pronation. (18,19)
The everted position of the first metatarsal seen in hallux valgus deformity is either due to torsion within the first metatarsal bone or due to pronation of joints located proximal to the first metatarsal. (20-22) This leads to the final dubious claim of all the rotational Lapidus procedures.
Claim #3: A Lapidus procedure which includes inversion rotation of the first metatarsal is necessary to correct all planes of the hallux valgus deformity.
From the Lapiplasty® internet site (2):
Lapiplasty® 3D Bunion Correction corrects the entire bone in 3D
Osteotomies target the cosmetic bump by cutting and shifting the bone in 2D, but do not address all 3 dimensions of the deformity or the unstable foundation.
From the LapiLock site (3):
Many surgeons often overlook the coronal plane rotation of the problematic metatarsal
FACT: While the new 3-D and 4-D Lapidus procedures target the first metatarsocuneiform joint to rotate the first metatarsal into inversion, scrutiny of the scientific evidence reveals that this joint is not the origin of pronation of the first metatarsal in HAV deformity.
Three studies, using simulated weight bearing CT imaging tracked the displacement of the bones along the medial column of the foot of patients with HAV deformity and healthy controls as the foot moved from an un-loaded to a fully loaded position. (7,8,23) These studies show that, at the first metatarsocuneiform joint, the first metatarsal was observed to move in the direction of inversion, dorsiflexion and adduction.
The rotational deformity of HAV seen at the first metatarsocuneiform joint is in the direction of INVERSION and rotating that joint further into inversion would seem counter-intuitive. See this weight bearing CT image of an HAV patient:

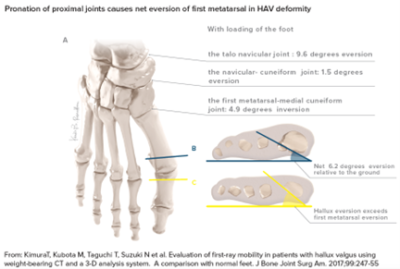 If inversion rotation of a joint were necessary to reduce pronation deformity in hallux valgus, then the surgeon would have to focus on the talonavicular joint, not the first metatarsocuneiform joint which is already inverted.
If inversion rotation of a joint were necessary to reduce pronation deformity in hallux valgus, then the surgeon would have to focus on the talonavicular joint, not the first metatarsocuneiform joint which is already inverted.
Kimura showed that in patients with hallux valgus, the actual pronation deformity originates at the talonavicular joint, not the first metatarsocuneiform joint.(8) With loading, the study authors observed the following bone segments to rotate in this magnitude and direction:
-
the first metatarsal moves 4.9 degrees into inversion;
-
the medial cuneiform moves 1.5 degrees into eversion;
-
the navicular moves 9.6 degrees into eversion; and
Conclusion: The net motion of the entire medial column results in 6.2 degrees of eversion and this motion originates in the talonavicular joint, not the first metatarsocuneiform joint.
Claim #4: Patients are told that all other bunion procedures have a high failure rate.
From the Lapiplasty® site (2):
“70% of bunion patients may have their bunion return over time”
“1 in 3 patients are dissatisfied after osteotomy bunion surgery”
FACT: A review of all published research shows a low recurrence rate and high patient satisfaction with all types of bunionectomy surgery.
The statements about high recurrence and low satisfaction with standard bunion surgery found on the Lapiplasty® internet site cites one study of 77 patients which was published from a single institution in Finland. (24) What is not cited is a high level study published in the most prestigious orthopedic surgery journal in the world. Barg and co-workers conducted a systematic review of 229 studies of all common types of hallux valgus surgery published in the medical literature. (25) Dissatisfaction with the results of surgery in 12, 866 patients was 10.6%. Residual pain in the great toe joint was found in only 1.5% of patients. More important, the rate of recurrence of hallux valgus deformity across all types of surgical procedures was 4.9%.
Concluding remarks:
Promoting medical technologies on the internet can be an effective and constructive method of patient education. Many companies, including my own, feature educational tabs on their websites in order to provide an overview of scientific research in a simplified and meaningful format for the lay public to interpret. Touting new insights and theories supporting innovative technologies is perfectly acceptable as long as there is sound science supporting the claims.
Conversely, posting distorted information criticizing current medical and surgical practice creates confusion among patients and spurns distrust of practitioners who make decisions based upon peer-reviewed research and clinical experience.
REFERENCES
-
https://andrewlundquist.substack.com/
-
https://www.lapiplasty.com/
-
https://lapilockbunionsurgery.com/?radius=25
-
Coughlin MJ, Jones CP .Hallux valgus and first ray mobility. A prospective study. J Bone Joint Surg Am. 2007; 89(9):1887–1898.
-
Shibuya N, Roukis T, Jupiter DC. Mobility of the first ray in patients with or without hallux valgus deformity: Systematic review and meta-analysis. The Journal of Foot & Ankle Surgery. 2017; 56 :1070–1075.
-
Faber, FW; Kleinrensink, GJ; Verhoog, MW; et al.: Mobility of the first tarsometatarsal joint in relation to hallux valgus deformity: anatomical and biomechanical aspects. Foot Ankle Int.1999; 20:651 – 656.
-
Geng X, Wang C, Ma X, Wang X, Huang J, Zhang C, Xu J, Yang J. Mobility of the first metatarsal-cuneiform joint in patients with and without hallux valgus: In vivo threedimensional analysis using computerized tomography scan. J Orthop Surg Res 2015;10:1–7.
-
KimuraT, Kubota M, Taguchi T, Suzuki N et al. Evaluation of first-ray mobility in patients with hallux valgus using weight-bearing CT and a 3-D analysis system. A comparison with normal feet. J Bone Joint Surg Am. 2017;99:247-55
-
Munuera PV, Dominquez G, Polo J, Rebollo J. Medial deviation of the first metatarsal in incipent hallux valgus deformity. Foot Ankle Int. 2006; 27, 1030-1035.
-
Sanders, AP; Snijders, CJ; van Linge, B; Medial deviation of the first metatarsal head as a result of flexion forces in hallux valgus. Foot Ankle. 13:515 – 522, 1992.
-
Snijders CJ, Snijder JG, Philippens MM. Biomechanics of hallux valgus and spread foot. Foot Ankle. 1986;7:26-39.
-
Dayton P, Feilmeier M, Kauwe M, Holmes C, McArdle A, Coleman N. Observed changes in radiographic measurements of the first ray after frontal and transverse plane rotation of the hallux: does the hallux drive the metatarsal in a bunion deformity? J Foot Ankle Surg 53:584–587, 2014.
-
Dayton P, Kauwe M, Feilmeier M. Clarification of the anatomic definition of the bunion deformity. J Foot Ankle Surg. 2014;53(2):160-163.
-
Collan L, Kankare JA, Mattila K. The biomechanics of the first metatarsal bone in hallux valgus: a preliminary study utilizing a weight bearing extremity CT. Foot Ankle Surg. 2013;19(3):155-161.
-
Mahmoud K, Metikala S, Mehta SD, Fryhofer GW, Farber DC, Prat D (2021) The role of weightbearing computed tomography scan in hallux valgus. Foot Ankle Int 42:287–293.
-
Steadman J, Bakshi N, Arena C, Leake R, Barg A, Saltzman C. Normative distribution of first metatarsal axial rotation. Foot Ankle Int. 2021, 42(8) 1040–1048.
-
Najefi A, Zaveri A, Alsafi MK, Malhotra K, Patel S, Cullen N, Welck M. The assessment of first metatarsal rotation in the normal adult population using weight bearing computed tomography. Foot & Ankle International. 2021, Vol. 42(10) 1223–1230.
-
Campbell B, Miller MC, Williams L, et al. Pilot study of a 3-dimensional method for analysis of pronation of the first metatarsal of hallux valgus patients. Foot Ankle Int. 2018;39(12):1449-1456.
-
Conti MS, Patel TJ, Caolo KC, Amadio JM, Miller MC, Costigliola SV, Ellis SJ, Conti SF. Correlation of different methods of measuring pronation of the first metatarsal on weight bearing CT scans. Foot & Ankle Int. 2021; Vol. 42(8) 1049–1059.
-
Ota T, Nagura T, Kokubo T, et al. Etiological factors in hallux valgus, a three-dimensional analysis of the first metatarsal. J Foot Ankle Res 2017;10:1–6.
-
Cruz EP, Wagner FV, Henning C, Sanhudo JAV, Pagnussato F, Galia CR. Does hallux valgus exhibit a deformity inherent to the first metatarsal bone? J Foot Ankle Surg. 2019;58(6):1210-1214.
-
Randich JR, John JK, Gomez K, Bush W. Frontal plane rotation of the first ray in hallux valgus using standing computerized tomography (CT). Jour Foot Ankle Surg. 2021; 60, 489-493.
-
Watanabe K, Ikeda Y, Suzuki D, Teramoto A, Kobayashi T, Suzuki T, Yamashita T. Three-dimensional analysis of tarsal bone response to axial loading in patients with hallux valgus and normal feet. Clin Biomech 2017;42:65–69.
-
Pentikainen I, Ojala R, Ohtonen P, et al. Preoperative radiological factors correlated to long-term recurrence of hallux valgus following distal chevron osteotomy. Foot Ankle Int. 2014; 35(12):1262-1267.
-
Barg A, Harmer JR, Presson AP, et al. Unfavorable outcomes following surgical treatment of hallux valgus deformity: a systematic literature review. J Bone Joint Surg. 2018; 100(18):1563-1573.




